By Sara Anderson, Executive Director
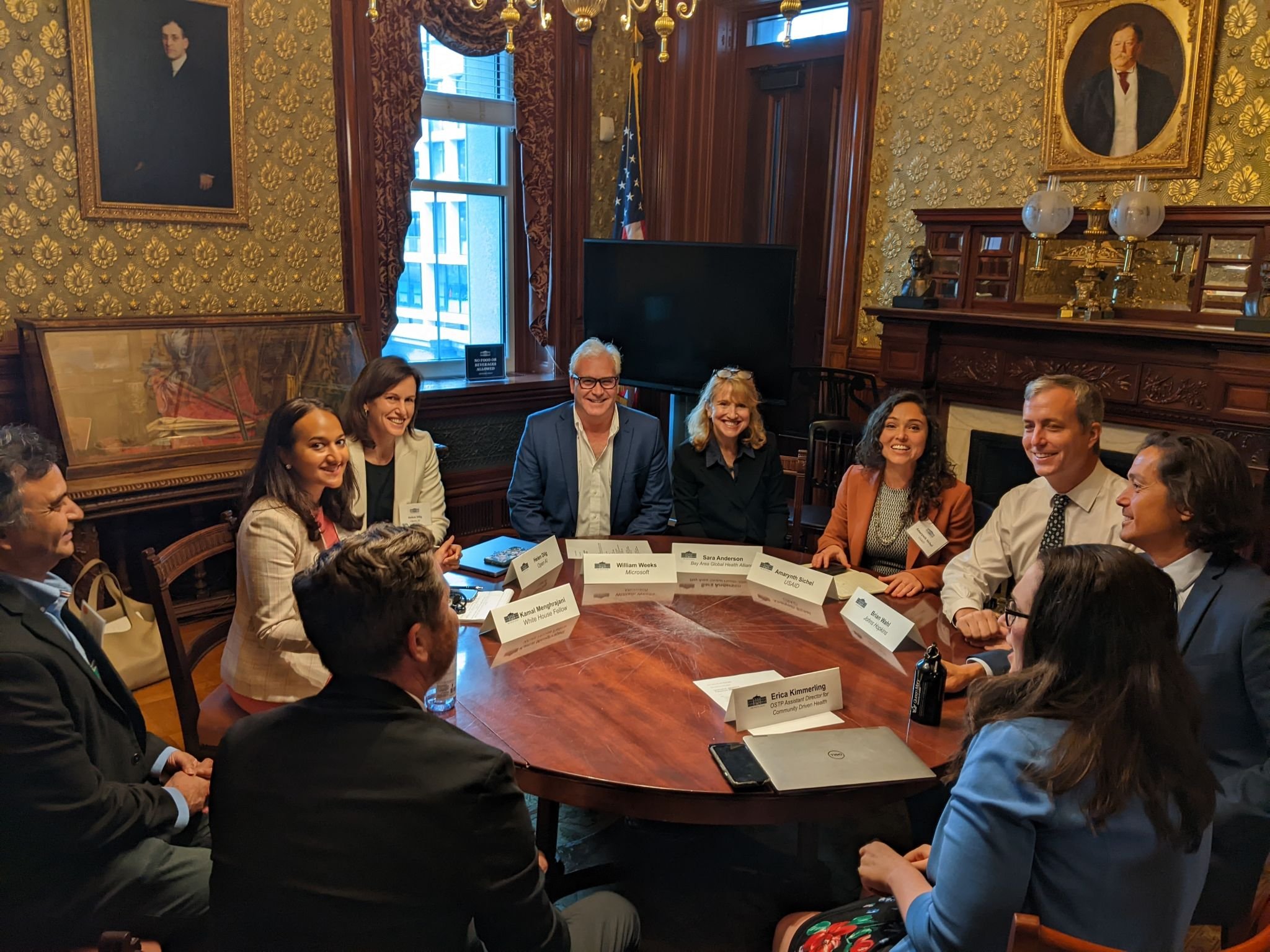
Last week, I was honored to be part of the White House Roundtable on AI and Health. The White House Office of Science and Technology Policy convened a distinguished group of leaders from across sectors to discuss how artificial intelligence (AI) can be safely deployed to improve health outcomes, with a special breakout session on the use of AI to improve public health and global health. To prepare for the meeting, I sought input from our multi-sector members and key stakeholders on what points they would make if they were at the table.
Here are the ABCs of what’s important to the Bay Area Global Health Alliance about AI & global health.
A. Access: Ensuring accessibility in low-resource areas and for underserved populations is essential. Policies and initiatives should prioritize equitable AI technology access to bridge health disparities. Low- and middle-income countries (LMICs) stand to gain the most from AI in healthcare but risk widening health disparities without proper investments and proactive planning. “As you get excited about these shiny, sexy AI tools, don’t forget about those at the base of the pyramid who do not have connectivity,” cautioned Alliance Board Member Natasha Sunderji, managing director, Accenture ADP. “Regardless of what exciting solution you create, you will leave them behind.”
B. Basics: AI’s usefulness in global health depends on the same basic building blocks needed for robust digital health systems — connectivity, interoperability, smartphone penetration, high-quality data, digital literacy, workforce capacity building, financing, governance, and standards — and that infrastructure is still lacking in many LMICs. The fundamentals in digital health need to be the foundation in AI and health, in alignment with the broader principles and best practices for digital health that have been developed. Could the excitement around AI help drive investments in the basic digital health building blocks?
C. Community-Driven: AI solutions must be carefully tailored to local communities’ unique needs and contexts to avoid exacerbating existing health disparities. They also must be driven by local governments and stakeholders in LMICs to align with their priorities and address their health challenges. Importing tools from high-income countries without local co-creation doesn’t work. “Robust community engagement in AI design and deployment helps ensure sustainability and reliance on community resources and capabilities,” wrote PATH, under the direction of Dykkie Settle, Chief Digital Officer.
D. Data: Data privacy and safety are of utmost priority, and addressing data access, biases, and trust are also key issues. Collaborative efforts between governments and regulatory authorities are crucial for establishing and reinforcing robust data privacy and ethics regulations, with citings of General Data Protection Regulation (GDPR) as a good model. Investments are needed for inclusive data representation (especially from LMICs) to train AI models to mitigate biases and improve the accuracy of AI-driven healthcare solutions. Low electronic medical record (EMR) adoption rates, estimated at less than 40% in LMICs, hamper the ability to aggregate historic and real-time patient data, according to the USAID Center for Innovation and Impact’s AI and Global Health report. Building trust through community engagement, transparency, and rethinking data ownership is vital for successful AI-driven healthcare solutions. Accenture’s 2022 Tech Vision research found that only 35% of global consumers trust how organizations are implementing AI.
E. Equity: AI has the potential to bridge existing equity gaps, if we start with equity as a foundational principle. “Without careful oversight, leadership, and regulation, equity divides will grow within and between countries, amplifying existing social and economic inequities,” wrote the WHO Digital Health and Innovation team, led by Alain Labrique. We must create a sustainable ecosystem that fosters inclusive innovation in AI and support government staff and private sector entrepreneurs with the knowledge and skills to effectively develop, regulate, and utilize AI technologies.
F. Framework Transformations: In global health, we’ve traditionally focused on disease-specific approaches, leading to fragmented health systems with data challenges. AI allows us to shift and focus AI as a horizontal disruption across the multi-sector health ecosystem. Policy iImplications differ between vertical and horizontal interventions, necessitating considerations for fairness, innovation, adaptable policies, and norms to address diverse interests. Existing regulation, oversight, management, and implementation structures may not be well suited to advance AI tools. New cross-sector collaborations and public-private partnerships may be needed for a robust ecosystem with equity at its core.
G. Governance: To ensure equitable AI benefits globally, we must address governance gaps, public trust issues, and ethics. Unregulated AI risks widening social and economic disparities. We must bolster local government-led regulations for swift, standardized validation of AI tech in health systems, which is the focus of HealthAI’s strategy. In addition, the “go fast, break it” start-up mentality of tech must be curbed by the ethical expectations of healthcare; lives are in the balance. Policymaking also needs to “keep up” with foresight on where things are heading in five years and start creating policy now to address; misinformation and disinformation are already rampant and wreaking havoc on public health. Lastly, we need to prioritize what will have the most significant near-term impact on the greatest number of human lives and use AI for resource optimization first, recommended Brittany Hume Charm of Pendulum and cited by others.
At the OSTP listening session and roundtable, there was substantial alignment and echoes of our members’ priorities on many of the risks and opportunities before us at this pivotal moment. Here’s their official read-out.
I’m grateful for the input and exceptional expertise in the Bay Area Global Health Alliance’s network. More than a third of members are focused on digital health technology. Special thanks go to the WHO Digital Health and Innovation team, UC Berkeley Haas School of Business, AIfluence, Abt Associates, Accenture ADP, Baraka Impact Finance, Cepheid, Gilead, Google, I-DAIR, Mastercard, Merck for Mothers, McKinsey, Patrick J. McGovern Foundation, Nivi, PATH, Pendulum, Reach Digital Health, Roche Diagnostics, Stanford Biodesign, Upswell, and YLabs. And thanks to OpenAI’s ChatGPT for helping summarize my 30+ pages of notes.